
- Important
- How I got my “Yes”
- My First Appointment
- My Second Appointment
- The Phone Call
- Between The Beginning Of Your Journey To Now
- Surgery Day!
- Follow-up Appointment
- The Results
- What Do I wish I Had Known?
- CheckLists
- TLDR;
- FAQ
Important
This blog entry goes into detail describing the process I went through to have Tubal Ligation Surgery. It also touches on LGBTQ+, Polyamory, and abortion. Comments that are not respectful will be deleted.
Please be aware that the artwork provided in this entry was created by me and does not come from a medical journal.
What is Tubal Ligation Surgery? (a Real medical resource)
How I got my “Yes”
In 2017 I finally got the “YES” I had been trying to get for 11 years of my life. Well- Almost. For those 11 years, I had been trying to get permanent birth control in the form of a hysterectomy and had heard a repeated “NO” from at least 3 different family doctors.
This is the story of how I got my “YES,” what the process was like, and any information I can provide to help others like me. This occurred in Alberta, Canada when this surgery was free through coverage by the province, so mileage may vary. I’ve found myself sharing my Facebook Album covering the events so often that a goal of this “Sketchbook Journal” was to document this process in a much more shareable and readable way. You also get some casual notes because this is also a personal record for myself. So, here we go.
After going to my doctor because I had stomach issues I heard the words I had tried hard to never hear in my life.
“Congratulations, you’re pregnant.”
I had gone to the doctor with stomach pains and other symptoms that, admittedly, synced up with my diagnosis, but it didn’t occur to me because I had been using the Depo shot and hadn’t had any issues in about 4 years. Hell, I had barely had a period in 4 years, which… is another conversation.
The ensuing conversation was exactly what you’d expect when your response is “Great, please book me in for an abortion.” The man standing before me was not my doctor, but a new doctor in orientation, and he absolutely failed at how he handled this appointment. I asked for MY doctor so that we could discuss the situation, which is when he finally gave in and brought me the information for booking an abortion, and explained that the process required me to do it.
This is important because it was during the counselling session before my abortion that it was brought to my attention that while a hysterectomy was not normally recommended for someone my age because of the issues it can introduce (early menopause for one), a tubal ligation would also help me reach my goal of not having children without having to remember birth control pills or take a BC method that disagreed with me (the depo shot). She agreed to refer me to a doctor to move that process forward, but that’s not actually how I got there.
It was during the follow-up with my actual family doctor for the abortion that I asked if he could check on the referral because I hadn’t heard anything. He didn’t even know about it, so we decided to move forward on a referral to his usual expert, with his newfound motivation provided by my abortion, and request for a tubal ligation – technically a reversible procedure.
Ironically, I finally heard from the referral that came from the abortion clinic the night before my surgery. It was MONTHS faster to go through my family doctor.
My First Appointment
In December 2017 I had my first appointment with a local obstetrician and gynecologist.
As a person who does not want children, I did not quite understand what that would mean when I walked into the office. The first thing I would warn a person about is that if you have that combo of specialists you will be walking into an office full of pregnant people and baby photos on the wall. That might be a given, but I hadn’t learned much about my doctor yet and was not expecting this and it could be triggering depending on your circumstances. Especially if the moms are talkative and curious.
It is okay to tell them it’s personal and you do not feel comfortable sharing why you are there. Your desire for privacy and safety is valid. As someone looking to get this procedure without having children we know how often people disrespect that choice.
Office intake was easy. I filled out a general intake form with the normal healthcare information they usually ask at appointments in offices where you are new. This includes allergies, medication, and in this case – any relevant reproductive information. Once they were ready to seat me in a room they took my height and weight.
My entire appointment only lasted 15 minutes. I met my surgeon and he asked me why I wanted to get my tubes tied. I explained that I had been pregnant and did want kids BEFORE that happened, and I still did not want kids. My quick frustration with his follow-up questions was enough to convince him I knew what I wanted, so he began explaining the surgery.
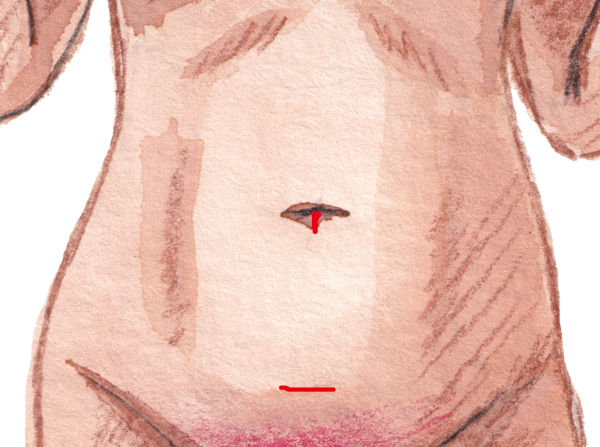
The total surgery would take 15 minutes. They would put me to sleep for it and make 2 incisions, both roughly 1″ in length. The first was in my belly button to insert the camera they would use to see everything, as well as a gas tube to expand my tummy to make that easier to do, and the second would be above my Uterus to gain access to my Ovaries.
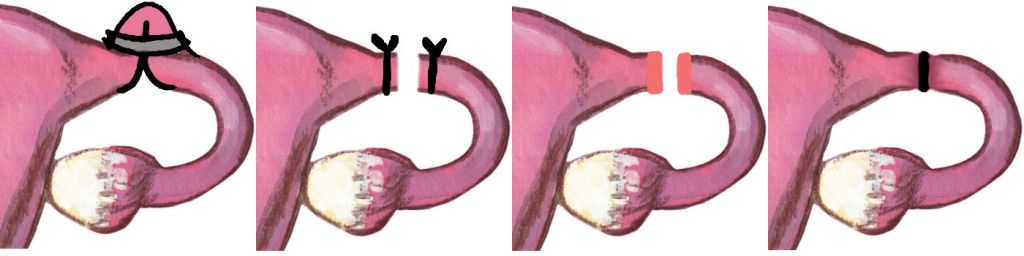
After that, they would clamp my fallopian tubes shut with a clamp similar to the “Clipped” example below. This means that if I ever change my mind (nope) I could likely have the clip removed and after some healing still be fertile. But, aside from some exceptional situations, I should otherwise have permanent birth control after this surgery. It was also a day surgery, so I would also likely get to go home that same day.
It’s that simple.
My doctor explained that in some rare cases, the fallopian tubes can grow around the bands, heal back together, or even grow around the cuts, but that is very unlikely to happen. To make sure everything healed the way that it should I should take it easy for 10 days, but my doctor was only able to excuse me for 7 days from work, in which 2 of those initial days I would not be allowed to drive.
He also expressed concern about getting me booked in the hospital because they usually only accepted women with at least 2 children as they are a Catholic hospital, but by the time I had left the appointment, the receptionist had already successfully booked me a time at the hospital for January 10th, 2018, a very welcomed early birthday present. However, I had to return in 1 week to fill out paperwork.
My Second Appointment
The second appointment was more about the things my surgeon, his team, and the hospital would need to know. They had me sign a waiver for the hospital, a form stating I had someone to properly care for me after the surgery (my partner), and more documents covering similar medical information to the office’s required medical information. I provided them information about my allergies, and pre-existing health conditions such as depression, anxiety, sleep apnea, and psoriasis. Nothing is too small or not worth mentioning. I never learned until years after this event that Psoriasis is actually an immune system disorder, which is a lot more dangerous than just dry skin.
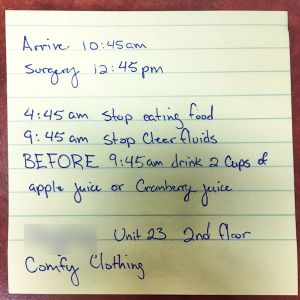
My doctor explained that a day or two before the surgery I would get a phone call with instructions for the night before. Following those instructions was important or they would not be able to perform surgery. A sheet of paper explained that I would have to eat a light snack before fasting for 8 hours and provided a small list of recommended foods. I would also have to drink 2 glasses of juice 3 hours before surgery.
He also covered what might happen after the surgery. It was expected that I would be tired for a couple days due to the medications used to knock me out and keep me from feeling pain. We also booked a follow-up appointment for 16 days after surgery.
What I wish he had explained was that I might feel pain around my shoulders as the gas used to expand my stomach has a tendency to migrate up to that area before being expelled from the body.
The Phone Call
I actually got 2 phone calls. The first was registration information. I didn’t write down what that meant, but I’m sure it’s basics like name, birthday, and basic identification information. The second call gave me instructions for surgery day. My arrival time, surgery time, when to stop eating food, when to stop clear fluids, when to drink my two cups of juice, and what kind of juices I could choose from (Apple and Cranberry). They also told me where to sign in and to wear comfy clothing as I would be there for a while.
Between The Beginning Of Your Journey To Now
This might be one of the more important sections of this entire post.
You need to know your decision is valid and you deserve to make this choice for yourself no matter what anyone tells you.
From the moment I started dating until before I started this journey, I thought I was SO OVER people telling me I was greedy for not wanting kids, or that I’d change my mind.
Once I confirmed I was doing this and had a surgery date to talk about, the people telling me these things doubled down on me. For an entire month, a co-worker told me I’d regret it every single time she saw me. The day before surgery everyone I saw in person tried to talk me out of my surgery, while online all of my friends were super supportive. I would like to take this moment to say though, that my parents, brother, and partners were incredibly supportive.
This is your choice. Only you know what you want.
At the time of writing this it has been 7 years since my surgery and I do not regret it even a little bit. I have never looked back. My partner and I are happily married, I am still my weird pansexual, polyamorous self, and I have protected myself from a future I do not want to the best of my abilities. It was one of the best decisions I have ever made.
Surgery Day!
Morning Prep
Day-of was exciting! I woke up at the crack of dawn excited like it was Christmas! … except earlier because sunrise is like 9am in January and I was definitely getting some food in me before my cut-off time of 4:45am.
My boyfriend was less thrilled about waking up early, but he was great and got up with me since he already planned on spending the day with me at the hospital.
I recommend having a shower first thing in the morning and then putting your favourite comfy clothing on. You will be sitting in a hospital waiting room, bed, or change room, or wherever you need to be for a long, uncomfortable, and cold period of time. You may not always be wearing it, but when you aren’t you’ll get to look forward to putting it back on. A blanket for the waiting room may also be a good idea after you change into your gown if they don’t have a room for you immediately. Uncomfortable chairs and thin material with exposed legs are not a good combination. You should also definitely bring something to do, whether you bring your Nintendo Switch, a good book, or even just your phone – but maybe bring an external power bank just in case. My phone died quickly because we were so deep in the hospital that it kept trying to find a connection.

Something I wish I had thought of was that I would be walking around in a hospital gown for a while. I care less about it today, but one of my regrets was that I did not shave anywhere from my belly button down that needed shaving before my surgery. That meant that I spent some time walking around the waiting room beforehand with my hairy Canadian winter legs out.
At The Hospital – Before Surgery
Once I arrived at the hospital it was a game of “hurry up and wait.” Though I was scheduled to arrive at 10:45am my surgery was not for another 2 hours. Most of this was spent sitting in the waiting room after I signed in. At some point they had me change into a gown and slippers (pictured above), but there was still some time between that and when I was actually taken for surgery
Once it was nearly my turn they assigned me a room, put me in a bed and wheeled me to a hall that was essentially parked beds waiting for the anesthesiologist to prep them and for the surgical team or anyone relevant to come around and speak to the patients. I spoke to my surgeon who introduced me to a student working with him that day, and my anesthesiologist.
I also got to overhear the guy beside me telling the person who asked him why he was there that he was in for a lobotomy and he absolutely made my day.

See this smiling face? This was the last time it smiled for the rest of the day. Why? Because 5 minutes after this photo the anesthesiologist tried to prep me for surgery and she couldn’t hit my vein. When I am dehydrated (which I was VERY dehydrated after fasting), my veins become practically invisible. She stabbed me about 15-20 times in each hand before she found one. They both bruised very badly and were sore for a couple days. The good news though, is that we were both from Newfoundland and nearby towns! So we got to joke around a little and relate to each other somewhat.
Once I made it into the operating room the anesthesiologist continued teasing me and complimenting my eyelashes to keep me distracted. I’m not sure how long it took her to actually release gas into my oxygen line, but I started out following their directions to scoot onto the surgery table, put my arms into the proper places, and while talking to the nurse I guess I blinked and that was it LOL.
At The Hospital – After Surgery
Though my surgery was over by 1pm I woke up in recovery around 3pm. My poor partner had been sitting in the waiting room the entire time.
As someone who has never had surgery before or after this I will admit that this was a bad time for me and I’ve been told it is not normally THIS BAD. Though I have been told I have a high pain tolerance (tattoos, electrolysis) I rated the pain I woke up with as an 8/10 for the nurse caring for me. She was… not kind or understanding. This was by far the worst part of the entire process for me. The pain was bad and uncomfortable enough that I was moaning and groaning without any control and the nurse’s response after initially giving me more pain meds was to “calm down” even though I understood what was happening and was actually quite calm. It just hurt. A lot.
Something I DID learn while being in a lot of pain, incapable of movement, but capable of clear communication was that a few beds away was another Pauline, who had just had the same surgery, and another person with the same last name as me. The nurses kept confirming my information throughout the day to be sure they were tracking information for the correct people, but it seemed excessive until I found this out. To be careful they moved the other Pauline into a different room because somehow they managed to book us into the same room to recover after we left the initial recovery room we were currently in.
An hour later I was wheeled back into my room for monitoring while my meds wore off. I was in and out of sleep for an hour or so while the nurse helped me monitor my pain level, nausea, and later my ability to walk. We continued to rate my pain level from 1-10 and after my initial recovery room experience it dropped significantly. It rated more around a 3/10. My nausea definitely picked it all up from here though. I began burping a lot, and while that helped a lot my nurse eventually gave me a needle with a liquid form of Gravol in it. When they felt I was nearly ready to leave they had me sit on the edge of the bed to gauge my balance. A little while after that they had me try to walk in a straight line, and then shortly after that they let me go home.
After The Hospital
My immediate directions for care after the hospital were to eat light foods with the suggestion of bread, avoid getting my stitches wet for a number of days, and take it easy for a while. My husband picked me up a Hot Chocolate and a donut from Tim Hortons, and my mom had already shown up at the hospital with a salad for me, expecting I’d have to stay overnight. So I was all set!
Home care involved mostly sleeping a lot, a heating pad on my stomach, pain meds prescribed by the hospital, and watching as much TV as I wanted for a week. Oh, I also moved my entire living room around while my husband wasn’t around. Don’t do that. You’ll regret it. That does not count as resting OR going easy on your body.
Things to Immediately be aware of
- The gas pain after my surgery lasted a few days.
- Walking and Gravol helped.
- Walking also sucked because it irritated my stomach.
- A heating pad is highly recommended.
- You will probably sleep a lot.
- When the medications wear off you may experience an emotional drop. Knowing this was a potential meant I was prepared for it to happen and I only struggled with it for about a day.
- Laughing is gonna suck for a while.
- Be Patient. Let Yourself Recover.
- Avoid being on your hands and knees for the first few weeks.
- You will have swelling in your stomach for up to 10 weeks.
- When they say do not have sex for the first 6 weeks – listen to them. (it won’t be difficult to listen)
Follow-up Appointment
My follow-up appointment actually kinda sucked, because I got there on time during a snowstorm only to find out my doctor was delivering a baby, so I ended up sitting in a crowded waiting room full of expecting mothers for 2 hours.
The follow-up appointment is actually pretty quick as long as everything is normal. My surgeon let me know that everything internally that he could see looked normal, my surgery went well, and he had zero concerns. When he inspected my incisions he noted some dry skin, but this is normal because I have Psoriasis. This happens when I am healing. If you do not have a skin condition like this and see dry skin absolutely point it out.
When I mentioned that I hadn’t had a period since the surgery I was asked to provide a pee sample, but this sample was never mentioned again, and I actually started my period that night.
Because I have some allergies to certain metals my doctor made me aware that they used a titanium clamp on each tube. He also mentioned he had heard I had been in a lot of pain afterwards and explained further about the gas. No one explained this to me previous to the surgery or even while I was in pain. When I expressed that I was in pain my friends on social media told me.
The Results
It has been 7 years since my surgery and everything went completely fine. My surgery was 100% effective and there have been absolutely 0 pregnancy scares!
What I did notice was that ALL of my period symptoms changed. While previously I had low cramps and some grouchiness, I now experience hard cramps, nausea, low iron, and some rough depression while nearing my period, and for a while it actually made my periods super short.
I have absolutely zero regrets when it comes to getting this surgery done. It has been peace of mind knowing that I won’t have to go through another abortion, put up a baby for adoption, or struggle with raising a kid I wasn’t expecting and did not want. Had I gone through with my pregnancy I would be dealing with a toddler during one of the scariest political moments of my life up to this point. Economically we’ve struggled, and as an LGBTQ+ person, I currently have a lot of concerns about my safety in the world. But I don’t have to have those worries for a child that I am in charge of.
What Do I wish I Had Known?
After getting my surgery I expressed displeasure in still having to deal with having a period. That was when I learned that another friend who had had the surgery had also had an Endometrial Ablation done at the same time. This had been offered to her, but not to me. This procedure will slow or completely remove your ability to have a period, which sounds great to me.
CheckLists
Finally, I wish I had had some resources. I’ve created some checklists below to use for your own surgery planning.
TLDR;
The secret to getting my tubal ligation was having an abortion, having a person who understood me refer me, having my doctor finally understand that I was truly dedicated to not having children, and 11 years of asking.
My initial appointments with the surgeon I was referred to required medical history I’ve added to the checklists above, and standing firm in my decision when he asked me questions. My medical history was required twice in two appointments because initially, it was for his office, and then it was for the hospital. He explained the process, which included putting me to sleep, cutting at the belly button for a gas tube to inflate my stomach and a camera so the surgeon could see, and a second incision above my uterus where the operation would actually happen. The doctor would place a clamp on my fallopian tubes, sew me back up, and the whole thing should take 15 minutes.
The surgery itself went exactly like that. But before I got to the surgery I had to shower, shave anywhere I didn’t want hair visible in a hospital gown, fast for 8 hours, drink 2 glasses of juice at a specified time, and then sit in the hospital waiting room for 2 hours waiting for my scheduled time. Once I was in a bed an anesthesiologist inserted a Cannula into my hand and they wheeled me off into the surgical room where my surgeon, a nurse, student, and the anesthesiologist worked on me.
I woke up 2 hours later with a lot of pain due to the gas used to inflate my stomach so they could see. This is normal and will make you gassy for a couple of days. An hour after waking up in recovery they moved me to my room where they monitored my pain, and nausea due to the gas, and let my medications wear off. Once they felt I was ready they had me sit on the edge of the bed, and then shortly after they confirmed I could walk straight and let me go home once I was ready.
Recovery was not as easy as it sounds like it should be for a day surgery. Day-of I could only eat light foods once I left. They recommended bread. For the next week, I stayed home, fell in love with my heating pad, and watched a lot of television. I followed a schedule for cleaning and rebandaging the incisions, had to keep them dry for a few days to avoid infection and avoid heavy movements like laughing or being on my hands and knees to reach things.
It’s been 7 years! I don’t regret anything! Woohoo!
FAQ
None Yet – Please ask questions below and I’ll add them here!

Leave a comment